Revision Total knee Replacement
Revision total knee replacement surgery is a procedure that replaces or repairs a previous knee implant that has failed due to wear, infection, loosening, or other complications. The decision to undergo revision TKR involves understanding the benefits, risks, and surgical nuances associated with this more complex procedure. Revision TKR is often much more complicated procedure than a primary TKR due to changes in the knee structure and the need for tailored implant choices and alignment strategies.
Surgical Complexity and Considerations
Revision TKR requires specialized planning and often more advanced techniques than a primary knee replacement. Dr Spelman will conduct a thorough evaluation, including imaging and tests to identify the underlying cause of the implant failure, as this will inform the specific surgical approach, choice of implant, and alignment strategy.
Indications for Revision TKR
Common reasons for revision surgery include:
- Implant Loosening: Over time, implants may become loose, leading to pain and instability.
- Wear and Tear: Polyethylene wear can cause bone and joint inflammation, sometimes requiring a new bearing surface.
- Infection: Infection in the knee replacement joint can necessitate removal of the existing implant and re-implantation.
- Instability or Misalignment: Improper alignment or ligament imbalance can lead to instability, pain, and limited function.
- Periprosthetic Fracture: Bone fractures near the implant may compromise stability and require a revision.
Advanced Techniques in Revision TKR
Due to the complexity of revision surgery, Dr Spelman utilizes advanced techniques and technology to optimize surgical outcomes, including robotic-assisted surgery, computer navigation, and specialized implant options tailored for revision procedures.
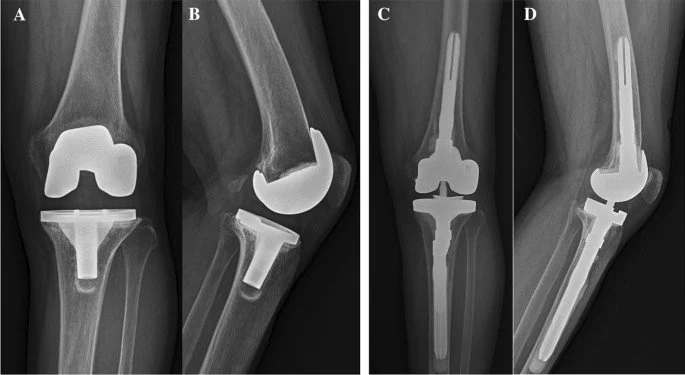
Implant Choice in Revision TKR
Revision TKR typically requires specialized implants designed to manage issues like bone loss, instability, and complex anatomy. Options include:
- Modular Implants: Modular designs allow for a tailored fit to accommodate individual bone deficiencies and ligament imbalances.
- Constrained Implants: These implants provide enhanced stability in cases of ligament deficiency or instability.
- Augments and Stems: Augments are used to fill bone defects, while extended stems offer additional support within the bone. Both components provide stability in areas affected by bone loss or implant loosening.
AOANJRR data underscores the importance of selecting implants with proven success rates in revision cases. Dr Spelman will recommend implants based on the specific requirements of each case, aiming to optimize both stability and durability.
Dr Spelman will carefully assess the implant and alignment strategy that best suits each patient’s specific situation, balancing the need for stability with functional outcomes.
Risks of Revision Total Knee Replacement
Revision TKR carries similar but elevated risks compared to primary knee replacement. These include infection, blood clots (DVT), implant loosening or failure, malalignment, fractures, and the potential need for further revision. Dr Spelman will discuss these risks with you in detail, ensuring a comprehensive understanding of both the potential benefits and challenges of revision surgery.
What to Expect from Your Revision TKR Surgery
Initial Consultation
Dr Spelman will conduct a thorough assessment of your knee, medical history, and prior TKR. Preoperative imaging, such as X-rays, CT scans, or MRIs, may be performed to evaluate the implant, bone quality, and joint structure. He will discuss both surgical and non-surgical options and answer any questions to ensure you are well-informed about the revision process.
7 Days Prior to Surgery
You may need to stop certain medications, including over-the-counter supplements like fish oil, as well as blood thinners if advised. Dr Spelman’s team and the anaesthetist will review your medication and medical history to prepare an optimal plan for surgery.
Day of Surgery
On the day of surgery, bring any relevant imaging studies to the hospital and adhere to fasting instructions. After preoperative preparations, you will proceed to the operating room for surgery, which typically lasts between 120 and 180 minutes, depending on complexity. After surgery, you will be monitored in recovery before moving to the hospital ward.
Day 1 Post-Surgery
Dr Spelman will evaluate your progress, and you will begin mobilizing with the help of a physiotherapist. Blood-thinning medications and compression stockings will be used to reduce the risk of blood clots.
Days 2-5
You will gradually increase your activity under the guidance of a physiotherapist. Pain management will be closely monitored, and most patients are discharged within 3-5 days, depending on mobility, pain levels, and available support at home. In some cases, patients may benefit from a short stay in a rehabilitation facility.
Week 2
You will have a follow-up appointment to check on the incision site, pain levels, and mobility. Many patients are using a walking aid at this stage, and any questions or concerns about the recovery process will be addressed.
Week 6-8
Dr Spelman will assess an X-ray of your knee to verify implant stability and positioning. Most patients transition to independent walking by this stage and may begin driving if cleared.
Ongoing Follow-Up
Regular follow-up appointments will be scheduled to monitor implant health and function, typically every 1-2 years depending on patient factors and surgical complexity.